A healthcare system’s strength is determined by its capacity to meet the needs of all population groups. In rural India, however, this strength is often undermined by inadequate infrastructure, a shortage of healthcare professionals, and significant financial barriers, leading to delayed or denied critical care access. Currently, initiatives like the National Health Mission are working to improve infrastructure, but the gaps persist. Strengthening health systems goes beyond building more hospitals or recruiting additional doctors. It requires creating a well-coordinated and responsive system that delivers timely, quality care tailored to the specific socio-economic and geographic realities of rural communities. This includes designing services that are financially accessible, culturally appropriate, and logistically feasible for populations that may lack transportation, digital access, or health literacy. Mobile health units, community-based health insurance models, and AI-powered disease surveillance tools have emerged as promising approaches to reach remote and underserved areas more effectively.
Why equity in rural healthcare cannot wait
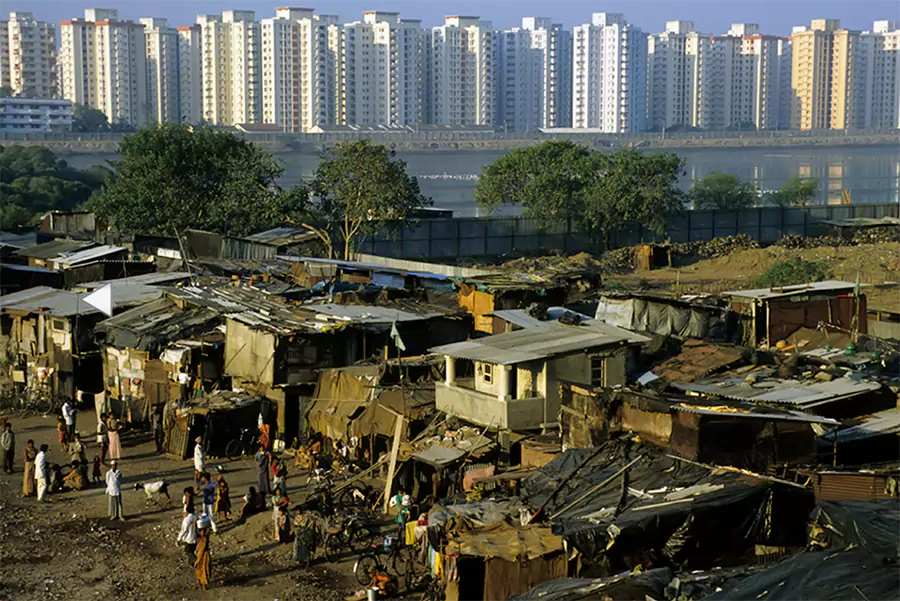
The World Health Organization (WHO) defines health equity as equal access to health resources while taking into account genetic, socio-environmental, and economic determinants.1 It means that everyone should have an equal chance to reach their best possible health regardless of their social or economic status. However, in India, the contrast between urban and rural healthcare access is glaring. Rural areas are home to 70% of the population, yet they are served by only 20% of the country’s doctors. In contrast, urban regions, with a much smaller share of the population, have access to 80% of the medical workforce.2 This imbalance extends beyond human resources. For instance, a 2024 study found that vaccination coverage in urban areas had reached 58%, while rural coverage lagged behind at just 39%. These disparities are compounded by financial barriers. Out-of-pocket health expenses push approximately 39 million people into poverty each year, and an additional 55 million fall below the poverty line due to healthcare costs.3,4 Addressing these inequities is an important step toward strengthening the overall effectiveness and reach of the country’s health care system.
Innovations expanding rural health access
Tackling inequity in rural healthcare requires more than just building new infrastructure. It demands the use of integrated tools and approaches that align with the lived experiences of underserved populations. Over the past few years, especially during and after the COVID-19 pandemic, several strategies have emerged that are making healthcare more accessible, accountable, and people-centred.
One such intervention is the use of mobile medical units and bank clinics. These initiatives bring healthcare services directly to remote and underserved communities, removing physical barriers that often prevent people from seeking care. In Chhattisgarh, mobile clinics have served 18 million people, conducting over 95,000 check-ups in just three years, with a strong focus on maternal and newborn care and immunization, as highlighted in a 2024 WHO report.5 This proactive approach has led to improvements in immunization rates, facilitated early detection of diseases, and increased access to basic healthcare services in previously inaccessible areas.
However, access to healthcare must also be accompanied by timely diagnosis. Screening and diagnostic services are crucial for early disease detection and better health outcomes. The integration of point-of-care diagnostic kits at Primary Health Centres (PHCs) and Health & Wellness Centres (HWCs) has played a key role in this regard. The Indian government has expanded the list of essential diagnostics to be offered at HWCs. The proposed National Essential Diagnostics List (NEDL) includes tests for conditions such as diabetes, malaria, tuberculosis (TB), HIV, syphilis, hepatitis B, thyroid function, and dengue, along with advanced imaging services like CT scans, MRIs, mammography, and echocardiography across different levels of care.6 This expansion has brought timely and accurate diagnosis closer to rural populations, enhancing the overall quality of primary healthcare.
Strengthening healthcare delivery also requires active participation from the communities it serves. Feedback and community monitoring mechanisms like the Village Health, Sanitation, and Nutrition Committees (VHSNCs) are vital in ensuring accountability. These platforms enable community members to be involved in health planning and service oversight. In Odisha, 83% of VHSNCs reported preparing village health plans, which is a strong indication of grassroots-level participation.3 This model of community monitoring fosters a sense of ownership and ensures that health services remain responsive to local needs.
At the same time, financial barriers continue to be a major obstacle in rural healthcare. Community-Based Health Insurance (CBHI) models offer a locally relevant and sustainable solution. While large-scale schemes like Ayushman Bharat are significant, CBHI models, especially those tailored for informal workers and self-help groups, can help plug coverage gaps. A notable example is the Self-Employed Women’s Association (SEWA) health insurance scheme, which provides comprehensive coverage through a combination of member contributions, subsidies, and service delivery partnerships.7 These models are effective in offering financial protection to communities that are often excluded from mainstream insurance schemes.
As healthcare systems continue to evolve, recent innovations in technology are creating new opportunities to close critical service gaps in rural areas.
Reimagining health systems with AI
While the government has made progress in expanding access to diagnostics and digital health infrastructure, the private sector has also contributed significantly through technological innovation. In particular, artificial intelligence (AI) and data analytics are transforming how healthcare is delivered in rural areas. These tools are being used to predict disease outbreaks, optimise resource allocation, and provide early warnings in epidemiology. Tricog Health, for example, collaborated with Maharashtra’s ST-elevation myocardial infarction (STEMI) program to use AI in analysing ECGs, detecting over 6,000 heart attack cases since January 2020.8 Similarly, deep learning algorithms are also being applied to improve the diagnosis of conditions such as tuberculosis and stroke through automated analysis of X-rays and CT scans. Tools such as these are especially valuable in rural areas that lack access to radiologists, and their effectiveness has been validated through large-scale clinical studies.9 These innovations help bridge the diagnostic gap, although challenges related to data privacy, algorithmic bias, and integration with public systems still need to be addressed.
These tools and interventions are not standalone solutions. They are part of a broader effort to build equity into the rural health system. When implemented in an integrated manner, they can effectively address not just immediate health needs but also the structural barriers that perpetuate healthcare inequities in rural India.
Barriers blocking rural health progress
While tools and interventions to strengthen rural healthcare exist, several systemic barriers continue to hinder progress. These challenges limit access, weaken service delivery, and place a heavy burden on rural communities.
- Low public health spending
Public health funding in India remains critically low, restricting the development of rural infrastructure and limiting access to essential services. In 2023, health expenditure was just 1.2% of GDP, placing India among the lowest globally.10 - Shortage of healthcare professionals
There is a severe shortfall of trained healthcare providers in rural India, leading to overburdened facilities and reliance on informal care. Although rural areas are home to over 65% of the population, they are served by only 34% of the country’s doctors.11 - High out-of-pocket expenditures
Healthcare continues to impose a heavy financial burden on rural families, pushing many into poverty. Around 92%of rural households pay for hospitalization directly from their own pockets, with chronic and emergency care causing the most strain.12
Pathways to build equitable and resilient rural health systems
To build truly resilient rural health systems, efforts must go beyond infrastructure development. Equity must be embedded in how care is funded, delivered, and governed. Achieving this will require a coordinated approach that brings together innovation, workforce strengthening, public-private collaboration, and deep community engagement. Below are five actionable areas where targeted reforms can make a tangible difference:
- Increase rural healthcare budgets and incentivize medical professionals
Allocate more funds to rural PHCs, HWCs, and district hospitals, while offering hardship pay, housing, and training incentives to attract and retain doctors in underserved areas.13 - Expand supply chains for affordable medicines through Jan Aushadhi Kendras
Strengthen the Jan Aushadhi network and logistics to ensure consistent drug availability in rural areas, and link them with PHCs and telemedicine services for wider access.10,14 - Leverage AI and data analytics for predictive healthcare interventions
Integrate AI and data tools into rural health systems for early diagnosis and outbreak surveillance, supported by investments in infrastructure, training, and data safeguards.8,9 - Strengthen multi-sectoral collaboration to scale successful interventions
Foster public-private and cross-sector partnerships to align local innovations with national goals and expand access to quality care through coordinated implementation.11 - Enhance training and digital literacy for frontline health workers
Upskill ASHAs and ANMs in using digital tools and diagnostics to boost rural service delivery and ensure technology reaches the last mile.12
The urgency of investing in equitable rural health systems
Equity must be at the heart of rural health systems strengthening in India. Addressing longstanding gaps, be it infrastructure, medical workforce, or financial protection, requires more than isolated interventions. It calls for integrated solutions rooted in innovation, community engagement, and policy support. Mobile medical units, AI-powered diagnostics, and community-based insurance schemes show promise, but their impact hinges on sustainable funding, capacity building, and inclusive governance. Public-private partnerships and greater investment in digital training for frontline workers are essential to strengthen health systems in rural India. India’s rural health systems can no longer be sidelined. A future-ready, equitable health ecosystem must not only address access gaps but also be rooted in community engagement, financial protection, and technological innovation. What we invest in today will shape the health outcomes of millions tomorrow.
- WHO. World Health Organisation. 2025 [cited 2025 Apr 6]. Health equity. Available from:
- Das S. Bussiness Standards. 2024 [cited 2024 Dec 4]. Rural India CHC’s see nearly 80% shortfall of specialist doctors: Govt rpt. Available from:
- Srivastava A, Gope R, Nair N, Rath S, Rath S, Sinha R, et al. Are village health sanitation and nutrition committees fulfilling their roles for decentralised health planning and action? A mixed methods study from rural eastern India. BMC Public Health. 2016 Jan 22;16:59.
- Prinja S, Bahuguna P, Tripathy JP, Kumar R. Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacol Toxicol. 2015 Dec 23;16:43.
- WHO. World Health Organisation. 2024 [cited 2025 Apr 6]. UHC-Partnership: Bringing primary health care to remote populations in Chhattisgarh, India. Available from:
- MoHFW. National Health Mission. 2019 [cited 2025 Apr 6]. Essential diagnostics at AB-HWC.pdf. Available from:
- Eze P, Ilechukwu S, Lawani LO. Impact of community-based health insurance in low- and middle-income countries: A systematic review and meta-analysis. PLOS ONE. 2023 Jun 27;18(6):e0287600.
- Pandey S. Mid-day. 2022 [cited 2025 Apr 6]. AI helps save over 6,000 at-risk heart patients in Maharashtra in past 2 yrs. Available from:
- John S, Abdulkarim S, Usman S, Rahman MT, Cresswell J. Qure Ai. 2023 [cited 2025 Apr 6]. Comparing tuberculosis symptom screening to chest X-ray with artificial intelligence in an active case finding campaign in Northeast Nigeria. Available from:
- Wadhwa M, Trivedi P, Raval D, Saha S, Prajapati H, Gautam R, et al. Factors Affecting the Availability and Utilization of Essential Medicines in India: A Systematic Review. J Pharm Bioallied Sci. 2024 Apr;16(Suppl 2):S1064–71.
- Zadey S. Global Health Now. 2021 [cited 2025 May 23]. Helping Doctors Reach Rural India | Global Health NOW. Available from: https://globalhealthnow.org/2021-02/helping-doctors-reach-rural-india
- Dutta SS. 92% of rural households’ hospitalisation costs are out of pocket, 77% for urban families—govt data [Internet]. ThePrint. 2024 [cited 2025 May 23]. Available from:
- J.,Vujicic M, Raha S, Bossert T. World Bank. 2010 [cited 2025 Apr 6]. Political economy of health workforce policy : the Chhattisgarh experience with a three-year course for rural health care practitioners. Available from:
- Department of Pharmaceuticals. Ministry of Chemical and Fertilisers. 2025 [cited 2025 Apr 6]. JANAUSHADHI. Available from:
- Dwivedi N, Bhargava N. World Economic Forum. 2022 [cited 2025 Apr 6]. Public-private partnerships can benefit healthcare in India. Available from:
- Rajput K. Empowering ASHAs with Digital Tools: Key to Transforming Rural Healthcare [Internet]. 2024 [cited 2025 Apr 6]. Available from: