In Parliament’s tumultuous monsoon session, focus briefly turned to the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana, with the presentation of a CAG report. It covers the implementation of PMJAY from its inception in 2018 to early 2021, which overlaps with my tenure as its founding CEO. Here I set the record straight on what I consider are misinterpretations in some media reports and suggest the future course for the scheme in light of the CAG findings.
Let us start with the good news. CAG report acknowledges that PMJAY “has had a strong positive impact on the economically weaker sections of society”. But the promise of PMJAY extends beyond its targeted population. It has provided a framework for universal health coverage, and has been used by seven states and UTs to expand coverage to their entire populations.
The rapid implementation and scalability of this large and complex scheme owe much to its innovative use of IT systems, which also helped CAG in conducting an in-depth audit. PMJAY is the first government scheme to intensively use artificial intelligence and machine learning techniques to prevent, detect and deter fraud and abuse. A state-of-the-art call centre that also served as a Covid helpline underscores PMJAY’s versatility.
There are also several areas that need improvement but let’s address a couple of red herrings first.
1) With regard to the headline exclaiming about more than 7 lakh Ayushman beneficiaries being linked to one telephone number, the primary intent behind collecting beneficiary phone numbers was to establish a means for patient follow-up. In the initial stages, the IT system lacked the provision to record cases without a phone number. Consequently, as a substantial number of beneficiary households lacked phones, either the default number ‘9999999999’ or alternative numbers were inputted by frontline workers.
The National Health Authority quickly recognised this issue and modified the software to validate phone numbers, if available, and otherwise recorded no phone numbers. So no systemic fraud or malpractice is necessarily indicated here. Indeed, the availability of all beneficiary information, including Aadhaar numbers, for public verification underscores the transparency of the programme.
2) Another sensational headline was that hospitals raised claims for people who were dead. The fact is that a small percentage of PMJAY patients do not survive. The hospitals raise claims in due course. All claims for mortality cases are duly audited before making any payments. Since hospitals have provided treatment to these patients, their claims are obviously entertained after due verification.
Ayushman Bharat’s success depends on effective monitoring, adaptability and a continuous commitment to refining its mechanisms. While continuous improvement based on the CAG report as well as on ongoing experience and feedback is needed, there are four fundamental challenges that the scheme must address head-on.
3) The first challenge is the database used for identifying beneficiaries. Just ask anyone familiar with the scheme, who is eligible for PMJAY? You will get a long and incoherent answer. The scheme relies on the 2011 Socio Economic Caste Census, an outdated database.
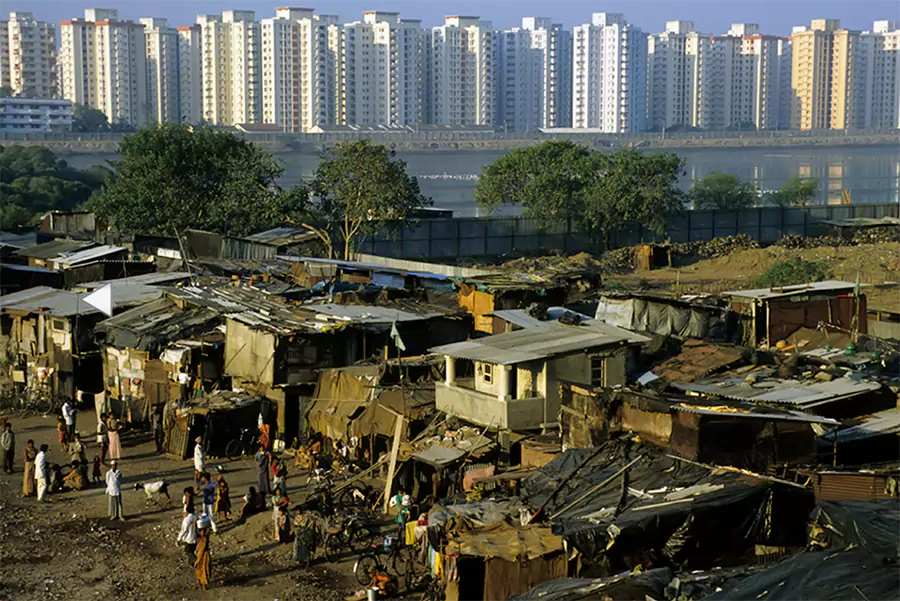
Complicated eligibility criteria, poor data quality and exclusion of a substantial number of the deprived population have created frustration among implementers and communities alike. In addition, PMJAY must consider the ‘missing middle’ – those not impoverished enough to qualify but not affluent enough for private insurance.
4) The second challenge is that the northern and eastern parts of the country do not have enough quality hospitals to address the pent-up demand that Ayushman Bharat seeks to release. Plus, many reputed private hospitals have not joined the scheme and some have withdrawn from it. Bringing all quality hospitals into the Ayushman Bharat fold is pivotal for the success of the scheme, as is promoting investments in quality hospitals in underserved areas.
5) The third challenge is the variance in implementation capacity and commitment to the scheme across states. In general, states with good health status have more effectively used Ayushman Bharat resources, thereby worsening the already existing inequalities among states. The CAG report has identified states that need focused attention.
6) Finally, PMJAY must intensify efforts to curb fraud and abuse. The scheme has been diligently proactive in pursuing fraudsters and ensuring stringent punitive measures.
Nevertheless, unscrupulous elements continuously devise novel ways to manipulate the system. Thus, it is imperative for PMJAY to pre-emptively strategise to outmanoeuvre them in this unseemly game of cat and mouse.
Ayushman Bharat isn’t any ordinary initiative; it’s a manifestation of our commitment to ensuring that quality healthcare is not a privilege for a few but is available to every Indian. Its early achievements illuminate the path forward, while its challenges remind us of the work that remains. By confronting these challenges, we can turn the promise of Ayushman Bharat into a lasting reality, making India ayushman for generations to come.
 Back to page
Back to page











Leave a Comment