1. You have extensive experience in designing and implementing international health programs, including community-based HIV/AIDS prevention programs and adolescent reproductive health projects in India. How do you see the initiative to digitalise healthcare, especially for women?
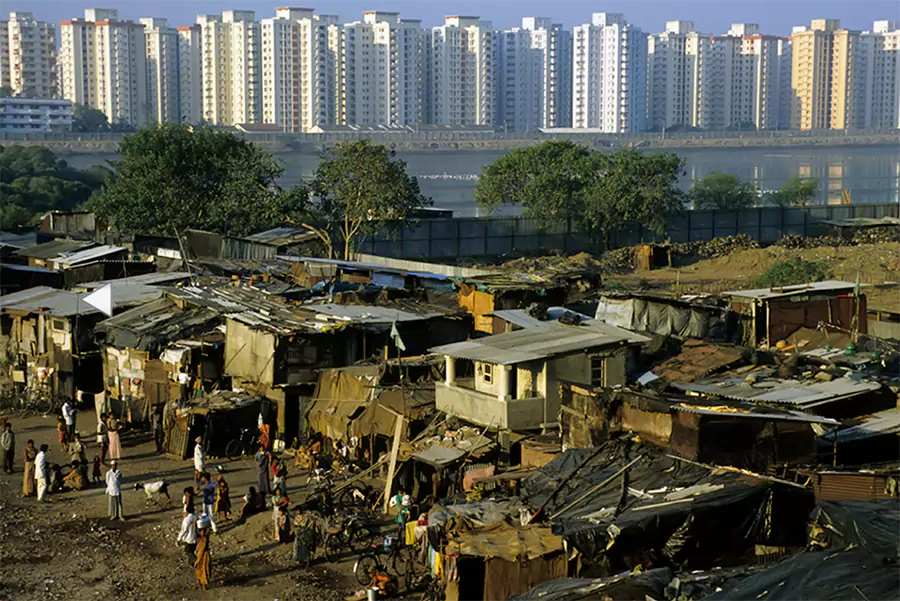
I have always believed that there is a great potential in digitalising healthcare. First, it will make information and services accessible for those who need it the most. Second, it will also support authentic data collection and evidence generation with more accuracy, than the current manual health management information system (HMIS). Digitalising healthcare across the spectrum of adolescent reproductive health, maternal and child health, nutrition and other health areas is vital. India has taken a great leap in this space where schemes began as early as 2015, where we have witnessed a transformation. However, with regards to data collection, it can become far more focused and analysed at various levels across numerous indicators. There is still some amount of information which can be distilled further. We need data that is more sex disaggregated, gender and rights based related, and which also looks at some qualitative nuanced indicators and parameters. Digital health interventions can have a transformational impact in the daily lives of women and girls. If Artificial Intelligence (AI) is carefully and ethically used, then it has the potential to improve health services and healthcare delivery till the last mile – which could be a game-changer. However, given that often the necessary safeguards are not in place, in many countries, the technology and digitalization can have a negative impact for the most vulnerable rather than the positive envisaged transformational potential.
Overall, yes, digitization in India has come a long way, but there are still a lot of areas where we can improve and use the data collected to safely strengthen implementation and reach the SDG goals.
2. You oversaw the PRACHAR Project in Bihar and an Urban Health Project based in Delhi which sought to promote behaviour change in and create positive impact on the reproductive health of adolescents and young adults. Could you share with us the factors – mental/physical/emotional and others – which causes hindrances in adopting healthy reproductive behaviour?
When we talk about hindrances in adopting healthy reproductive health (RH) practices, we should also look at maternal and child health and nutrition, because they are inter-linked with reproductive health. India’s deep-seated social norms, religious beliefs and practices cause many hindrances for individuals to adopt healthy RH practices. In my experience, understanding the genesis of these practices and beliefs, and engaging with the community while being empathetic and non-judgemental is crucial. Social and behavioural change communication (SBCC) efforts become successful when there is a balance between understanding the correct information and valuing it by the community and working towards creating an attitudinal change, which also considers the community’s beliefs, fears, practices, etc. Once the programme/project is successful in achieving the desired change (and this takes time), the focus then shifts to promoting consistency and continuity, among a critical mass. This then leads to a sustainable change. An example: Early ante-natal care (ANC) registration where pregnant women get themselves registered at a facility at the earliest and stick with the programme and system till they go in for institutional delivery, as well as opting for post-partum contraception, care of the new-born, etc. Similarly with contraception, if somebody begins using a particular method and remains consistent with that method, the percentage of failure gets reduced.
Additionally, catering to the demand for products and services among women and communities is also key. Unavailability of these products are also a big hinderance to adoption of healthy behaviours. Hence, there must be a balance between the demand and supply side interventions to bring about the desired behaviour change.
3. You were part of another project called “Sure Start” with PATH on reducing neo-natal mortality and promoting better maternal and new-born health outcomes. We would love to know more about that project as well as your experience on it.
Sure Start’s overall goal was to reduce neonatal mortality in select rural areas of Uttar Pradesh and urban areas of Maharashtra. There were different models used and the idea was to bring about behaviour change in the practices right from ante-natal care till postpartum, including neonatal and child health. This project worked on improved behaviour at the community level and focussed on antenatal and post-natal care. The BPCR (birth preparedness and complication readiness) checklist was used to make sure deliveries happen as per National guidelines, in a correct, hygienic and safe way, where the infants are healthier, and complications are reduced/prevented for both the mother and the new-born. After the baby is born, there are the first golden minute, golden hour, and golden day – which are extremely critical for their survival. Apart from some of the common causes of neonatal mortality, through our interventions, we realised hypoglycaemia was another cause because gestational diabetes in mothers was not being diagnosed at the correct time. Overall, it was important to ensure that the infants were being taken care of, not just clinically, but even at home with the support of ASHA, Anganwadi workers, and Auxiliary Nurse Midwives (ANMs); making sure of timely vaccinations, healthier breastfeeding practices, etc. But an important aspect under this project was the role that men or fathers can play to support mothers to make sure that their child has a great start right from the beginning. Male participation was critical for better health outcomes for the mother and child.
4. While working on adolescent and young adults’ sexual and reproductive health, on HIV/AIDS, and with refugees to help improve their quality of life, was there any instance(s) that deeply impacted you and is etched to your brain?
While working with refugees, I was both the medical and education councillor. Something that really impacted me was the realisation of what it is to leave not just your home, but an entire country behind and take refuge in a new country. For no fault of yours, you get completely uprooted and become a refugee. Few moments which are deeply etched to my heart include seeing people who led good lives in their own countries, now must attain a legal status of existence – elsewhere. This leads to extreme mental anxiety and despondency. I saw young girls injured and some boys/men with bullet wounds which led to them becoming paraplegic or hemiplegic. Young girls/women suffered trauma from sexual abuse, and you could see the wounds on their bodies. One lives through their trauma with them, which was quite horrific and scarring, both for us as counsellors and for their other family members.
While working with young adults on sexual and reproductive health, I realised how big a gap there is in our education system. Adolescents need the right information to prevent unintended pregnancies and STIs like HIV. I remember when I wrote my first module for adolescents between 15 to 19 years of age and the trainings we gave to over 30,000-40,000 adolescents in Bihar – seeing them take decisions which made a difference to their lives (in terms of reducing risky behaviour, delaying their marriages and improving their chances to have a better quality of life) felt soul enriching.
While working on HIV/AIDS, the most impactful realization was the kind of empathy people living with HIV/AIDS need. It was a startling realisation that people felt more for a woman who had only one sexual partner and it was her husband who made her positive. Whereas, for commercial sex workers, the narrative was different – after all, they were already in a risky business — hence were further stigmatized. Everyone needs to realise all people with HIV /AIDS, irrespective of their background, profession, or gender, need the same empathy, care and access to services and treatment – be it Antiretroviral therapy (ART), counselling, or support.
I also worked with young migrant girls from Jharkhand, who were made to work as domestic help in large cities. Their vulnerabilities and stories deeply impacted me. In their villages, they are duped by false promises of a better life and opportunities in big cities but then are brought in and are made to do household work. They are vulnerable to sexual harassment and STIs like HIV as well. The legal issues, unacceptability, and exploitation that they face, have an impact on their economical, emotional, physical, and mental well-being. A lot of these young girls get pregnant and go back to their villages. For various reasons including religious, they do not opt for abortion. They prefer to go through with the pregnancy and then give the baby away for adoption. The entire trauma that they go through pains me.
5. The theme for this year’s International Women’s Day was DigitALL: Innovation and Technology for Gender Equality. As we all know, COVID-19 has promoted the usage of technologies like telemedicine, usage of apps to book appointments. However, in a country like India with a significant digital gender gap, do you think digitalisation will boost access or become a hindrance?
Yes, I do see that digitalisation in the health sector will boost access of information. However, given the amount of fake news on social media, I would worry about the accuracy of this information. Another worry is the blind acceptance of the information without correct guidance or means to verify. With the kind of information we get, there is a certain amount of education and cognitive thinking needed to filter through and use what is needed. Before we even go to see a doctor, we already check online on what our symptoms mean for our health. Whether we talk about the urban educated or the rural population, who are semi-literate or are not literate, I would say digitalisation increases access, but I am not sure if the checks and balances are in place. In that context, I would say it is a hindrance.
Access to health care services will increase if we look at tele-medicine which has the potential to reach the last mile. The best example that I can give for digitALL would be the fact that today my female domestic workers have the ability to receive their salaries in the form of account transfers. However, while they know how to use UPI and the money transfer system, for many the payment still goes to the husband’s bank account. This is something we need to look at when we talk about digitalisation for gender equity.
In terms of accessing services, the most important thing in RMNCH+A will be the antenatal check-ups. Early registrations, institutional check-ups, postpartum check-ups, etc. are important. If WhatsApp or SMS alerts can go to individuals, it may increase the access.
6. Could you elaborate on respectful maternity care and why is it important to ensure its provision? According to you, can digital healthcare play a role in providing respectful maternity care in a country like India where 9,22,637 home deliveries were reported in 2021-2022?
During the COVID times, we did see an increase in home deliveries. Digital healthcare can play a role in not just providing respectful maternity care, but also quality care in terms of accessibility to specialists (tele-medicine). If proper guidance is given by specialists to the person performing the home deliveries, it will improve the quality of healthcare. We often see/hear of instances wherein there is little to no respect given to women at facilities, especially those run by the government. There are so many guidelines and protocols which are not being followed. Women need to be treated as human beings with dignity and respect, irrespective of the wealth quintile they hail from. India has released a Respectful Maternity Care (RMC) charter and guidelines have also been shared with health providers at all levels. Now, there is a need to see whether the RMC charter becomes a reality with all health workers and providers being trained accordingly and any woman from any background, irrespective of their caste and status, be treated with dignity which is their right.
7. Keeping in mind the vision for an efficient partnership between digital health and RMNCH+A, what would you think India should prioritise?
The vision for efficient partnership between digital health and RMNCH+A is where India should not just look at digitalisation from the point of view of data (it is equally important) but also improving the quality of information, security, and safety parameters, spreading outreach of that information, and improving the tele medicine facilities and other supply and demand related digital health facilities. Till all those things do not happen, digitalisation is not complete for me. Yes, digital health helps in maintaining data and it is very important for strategizing, but I think digitalizing should move to the next level. India should prioritise in collaborating and building appropriate partnership for health, the way it is doing for all the other digital tools. We have enough evidence to show that climate change has a huge impact on health including family planning, maternal health, and nutrition. Hence, the priority should be given to how do we coordinate with those efforts and make it a complete package.
A more comprehensive and interconnected way to digital health is the need of the hour.
8. Lastly, what do you think should be the responsibilities of different stakeholders to make digital inclusion a reality and ensure meaningful digital opportunities for all?
Central level think tanks and bodies are present to make the ease of doing business better in India- the startup culture, because of which we have numerous unicorns. In the same way, there are so many startups that have also emerged in the area of health. However, the ones I have seen are usually very product oriented, which is not wrong. But I think some of those platforms should look at a holistic way as well and smoothly move to the universal healthcare (UHC) mandate that India has initiated and make it into a reality.

Sita Shankar Wunnava is currently a freelance consultant in public health. She has over thirty-five years of experience with international health programs, including community-based HIV/AIDS prevention programs, gender programming and adolescent reproductive health projects in India. Her core competencies include designing, developing, and managing large public health and development programs; institutional capacity building, mentoring and team building; proposal development; developing training curricula and modules and action research; and monitoring and evaluation.
Sita’s past roles include Deputy Country Director at EngenderHealth; Director Programs at the Antara Foundation; Director, Maternal, Child Health and Nutrition, PATH India; Deputy Country Representative, Pathfinder International, India Country Office; Social Counsellor, UNHCR as well as consultancies with organisations such as Project Concern International and UNDP. She holds a Masters in Social Work from the Tata Institute of Social Sciences, Mumbai, and is a Bachelor of Arts from the Madras University, Chennai, India. She is also a Population Leadership Fellow from the University of Washington, Seattle, USA. She was a member of ICMR’s Expert Consultative Group on HIV/AIDS and is a member of the White Ribbon Alliance. Sita has also authored a chapter on ‘Innovative Simple Technology for Safe Motherhood’ in the book Safe Motherhood Initiative – the silent revolution published by PATH and FOGSI.